“Bites”, “Snacks”, & “Lunch” Communications for COVID-19 and COVID-19 Vaccines
Noni MacDonald and Eve Dubé
Noni E MacDonald1 and Eve Dubé2
Beyond masks, social distancing and handwashing, COVID-19 vaccines are a critical element in public health’s COVID-19 pandemic control strategy (1). However, COVID-19 vaccine acceptance is influenced by many contextual factors that are even more complex than the ones for traditional vaccines or even for the pandemic A (H1N1) vaccination campaigns (2). For example, there are high public expectations with COVID-19 vaccines. To complicate matters, there is a multitude of COVID-19 vaccines developed with differing platforms and approved through fast-tracked processes. Rates of efficacy and effectiveness also vary between COVID-19 vaccines, although it is not always easy to discern, as endpoints in trials differed. Equitable access to vaccines and the risk of potential serious adverse events following immunization are concerns for countries across the globe, including for varying target populations across the age span. Anti-vaccine activism about vaccine safety and effectiveness in the face of COVID-19 mutations is also a concern (3). These public issues have all generated much anxiety and stress, given how widely the pandemic has impacted health, well-being and the economy—globally, locally and personally.
The infodemic (i.e., an overabundance of information, some accurate and some not, both online and offline) that has flourished around COVID-19 has added stress and confusion for the public, health care providers and policy makers (4). In May 2020, the World Health Assembly passed a resolution concerning COVID-19 pandemic management focused on addressing the infodemic. This resolution called on member states to provide reliable COVID-19 content, take measures to counter misinformation (unintentional inaccuracies) and disinformation (deliberately false or misleading content), and leverage digital technologies across the response. The resolution also called on international organizations to address misinformation and disinformation in the digital sphere, to work to prevent harmful cyber activities undermining the health responses, and to support the provision of science-based data to the public. The Vaccine Misinformation Management Field Guide developed by UNICEF in December 2020 emphasizes the difference between misinformation (information that is false but not created with the intention of causing harm) and disinformation (information that is false and deliberately created to cause harm) (5). The latter is created and disseminated either for economic gain, or intentionally to deceive the public for political gain, prestige or attention. More importantly, misinformation and disinformation are “sticky”, travelling faster and farther than truth (6). The Organization for Economic Co-operation and Development (OECD) has emphasized four key actions that governments and platforms can take to address COVID-19 disinformation: 1) support a multiplicity of independent fact-checking organizations; 2) ensure human moderators are in place to complement technological solutions; 3) voluntarily issue transparency reports about COVID-19 disinformation, and 4) improve users’ media, digital and health literacy skills. This latter aspect is important for health care workers and those they advise.
Why do we fall prey to misinformation/disinformation?
Health decision making is complex, including decisions to accept vaccines; context matters, as does the specific vaccine in question (7). Social, cultural, historical and political factors influence how people feel and make decisions about vaccination. Furthermore, we are strongly influenced by what we think others around us are doing or expecting us to do, including people in social networks where disinformation is rife. We see causation in coincidences and see what we believe, rather than believing what we see; people prefer anecdotes and stories to data and evidence and pay more attention to negative information. This is why safety concerns and lack of trust may be especially prominent as the COVID-19 pandemic provides an ideal context for the spread of misinformation, disinformation and conspiracy theories, as they tend to arise in societal crises that generate increased stress, a sense of uncertainty, and increased concern for the future (8).
How can we overcome misinformation/disinformation in Canada?
The COVID-19 Vaccine Communication Handbook notes that achieving high COVID-19 vaccine acceptance levels requires context-specific and data-driven behavioural interventions, working at multiple levels supported by targeted communications with messages, tools, and techniques that help reach specific subgroups (9). At the community level, effective communication from public health needs to be proactive about COVID-19 and COVID-19 vaccines, not just reactive, as well as paying attention to traditional media reports and social media to detect misinformation that needs to be corrected.
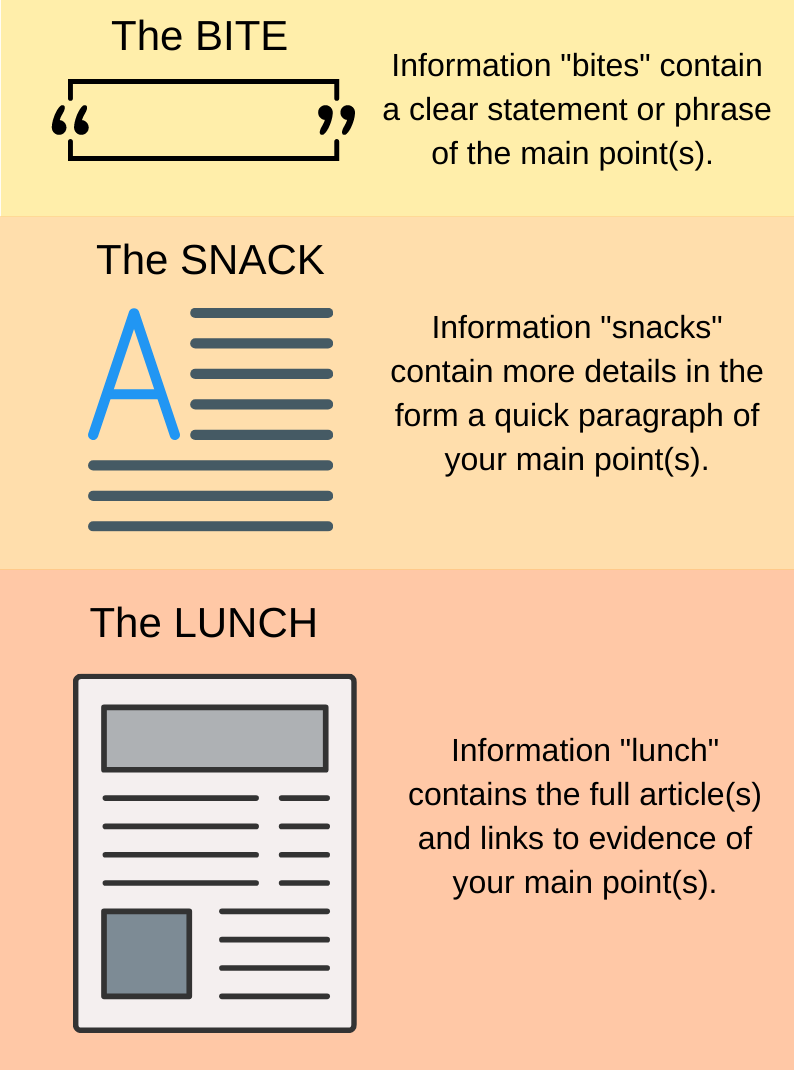
The communication analogy of “Bites”, “Snacks”, and “Lunch” comes in handy to help disseminate information in different formats. Some people want only a clear statement or phrase on the main point(s) of what to do (the information “bite”), while others want more details in the form of a quick paragraph (the information “snack”) – and still others want full articles and links to the evidence of the main point(s) addressed (the information ”lunch”). For the “lunch”, links to vetted evidence-based credible websites, such as those with a Vaccine Safety Net designation are helpful. When crafting communications, we need to remember the marketing principle that “data tells but stories are more likely to sell.” With the rapidly changing COVID-19 picture, linking the message to the local context and having it delivered or commented upon by known community leaders is key to enhancing credibility and stickiness.
Source: Canadian Public Health Association (CPHA), 2021
With respect to misinformation, correction will not lead to a backfire effect. More recent research has shown that the backfire effect is not as fixed as previously thought, and that it is important to correct the misinformation (10). Furthermore, there is research evidence to show that attitudinal resistance to misinformation can be conferred on the public and patients, by pre-emptively highlighting false claims, refuting potential counterarguments and unmasking the common techniques being used (i.e., fake experts, conspiracies, selectivity, impossible expectations, logical fallacies and misrepresentation – in other words, lies) (11) (12) (13). The United Kingdom has supported development and access to online browser games Bad News, Bad News Junior, and Go Viral, which teaches players how to become creators of disinformation and, in the process, strengthens their ability to detect and resist disinformation (i.e., avoid the con) (14). It’s Contagious!, It’s Infectious!, and Know It Or Not! are gamified educational experiences developed in Canada by the not-for-profit, Digital Public Sphere to help give people the opportunity to test their knowledge on common COVID-19 and vaccine misinformation narratives. A major building block to ensure the next generation will support immunization programs is the education of children and adolescents to become critical thinkers and science literate, so that they are able to recognize misinformation and understand the critical role vaccines have in health and well-being. Kids Boost Immunity is a helpful website developed in Canada, also now used in Ireland and Scotland, that has online lessons and quizzes to help children learn about immunization, cognitive bias, correlation versus causation and the scientific method, as well as about different vaccines, including COVID-19 vaccines.
What can health care professionals do?
Given that health care professionals’ advice and recommendations on immunization are very influential in a patient’s or individual’s decision to accept vaccines, it is critical that all health care professionals are well versed about the risks of the vaccine-preventable disease and the safety and efficacy of vaccines to advise their patients appropriately (15). This is especially important for COVID-19 and COVID-19 vaccines, given the infodemic raging. Health care professionals need to present these vaccines in a manner that shows their competence and caring to build trust, remembering that some only want a “bite”, while others want a “snack” or even a full “lunch” of information. Clear language, positive framing and motivational interviewing all have been shown to be helpful. Alerting patients to the power of disinformation, and teaching them how to recognize the con, are key in this period of information overload. The World Health Organization’s useful infographic on top tips for navigating the infodemic, the United Kingdom’s Bad News game, and the Canadian games, such as It’s Contagious! noted above, are helpful tools to share with patients. Health care professionals also need to speak up in family and social gatherings if misinformation and disinformation is being promulgated, as not speaking up sends the message that you, as a health care professional, agree with this false information. Finally, health care providers’ attitudes toward COVID-19 vaccines can be negatively influenced by misinformation or disinformation too. Given their important role in building and maintaining vaccine acceptance in patients, tailored strategies by public health and health care authorities to inform (“bites”, “snacks”, and “lunch” of information) and address health care providers’ concerns are also crucial. Critical thinking skills must be emphasized.
In summary, the COVID-19 pandemic will continue for some time. Public health and health care professionals need to be proactive and prepared to anticipate needs and concerns, to listen, and to update communication content and strategies when new data becomes available. It is important to beware of changing the context and how this may affect the way messages are interpreted by patients and peers. Remember that tailoring communication to fit the needs, concerns, level and amount of information needed – “bites”, “snacks”, and “lunch” – can help combat the infodemic, increase COVID-19 science literacy, and build acceptance of COVID-19 vaccines.
References
- Lockdowns and the COVID-19 pandemic: What is the endgame? Lytras T, Tsiodras S. 2021, Scandinavian Journal of Public Health, Vol. 49, pp. 37-40.
- Improving COVID-19 vaccine acceptance: Including insights from human decision making under conditions of uncertainty and human-centered design. Poland C, Matthews AKS, Poland GA. 2021, Vaccine.
- COVID-19 Vaccine: Critical Questions with Complicated Answers. Haidere MF, Ratan ZA, Nowroz S, Zaman SB, Jung YJ, Hosseinzadeh H, Cho JY. 1, 2021, Biomol Ther (Seoul)., Vol. 29, pp. 1-10.
- Ad hoc WHO Technical Consultation. Managing the COVID-19 Infodemic: a Call to Action. Geneva:World Health Organization, 2020.
- UNICEF. Vaccine Misinformation Field Guide. Guidance for addressing a global infodemic and fostering demand for immunization. New York: UNICEF, 2020.
- Science audiences, misinformation and fake news. Scheufele DA, Krause NM. 15, 2019, Proc Natl Acad Sci U S A, Vol. 116, pp. 7662-7669.
- Vaccine Hesitancy: Definition, scope and determinants. MacDonald NE and SAGE Working Group on Vaccine Hesitancy. 2015, Vaccine, Vol. 33, pp. 4161-4.
- Conspiracy theories as part of history: The role of societal crisis situations. van Prooijen J-W, Douglas KM. 3, 2017, Memory Studies, Vol. 10, pp. 323-333.
- Lewandowsky S, Cook J, Schmid P, Holford DL, Finn A, Leask J, Thomson A, Lombardi D et al. The COVID-19 Vaccine Communication Handbook. A practical guide for improving vaccine communication and fighting misinformation. 2021.
- Lewandowsky, S., Cook, J., Ecker, U. K. H., Albarracín, D., Amazeen, M. A., Kendeou, P., Lombardi, D. et al. The Debunking Handbook 2020. 2020.
- Inoculating against misinformation. van der Linden S, Maibach E, Cook J, Leiserowitz A, Lewandowsky S. 6367, Dec 1, 2017, Science, Vol. 358, pp. 1141-1142.
- Effective strategies for rebutting science denialism in public discussions. Schmid P, Betsch C. 2019, Nature Human Behaviour, Vol. 3, pp. 931-939.
- Inoculating Against Fake News about COVID-19. van der Linden S, Roozenbeek J, ComptonJ. 2020, Frontiers in Psychology, Vol. 11, p. 566790.
- Good News about Bad News: Gamified Inoculation Boosts Confidence and Cognitive Immunity Against Fake News. Basol M, Roozenbeek J, van der Linden S. 1, 2020, J Cogn, Vol. 3, p. 2.
- Unpacking Vaccine Hesitancy Among Healthcare Providers. MacDonald NE, Dubé E. 2015, EBioMedcicine, Vol. 2, pp. 792-793.